Understanding the Role of Butyrate
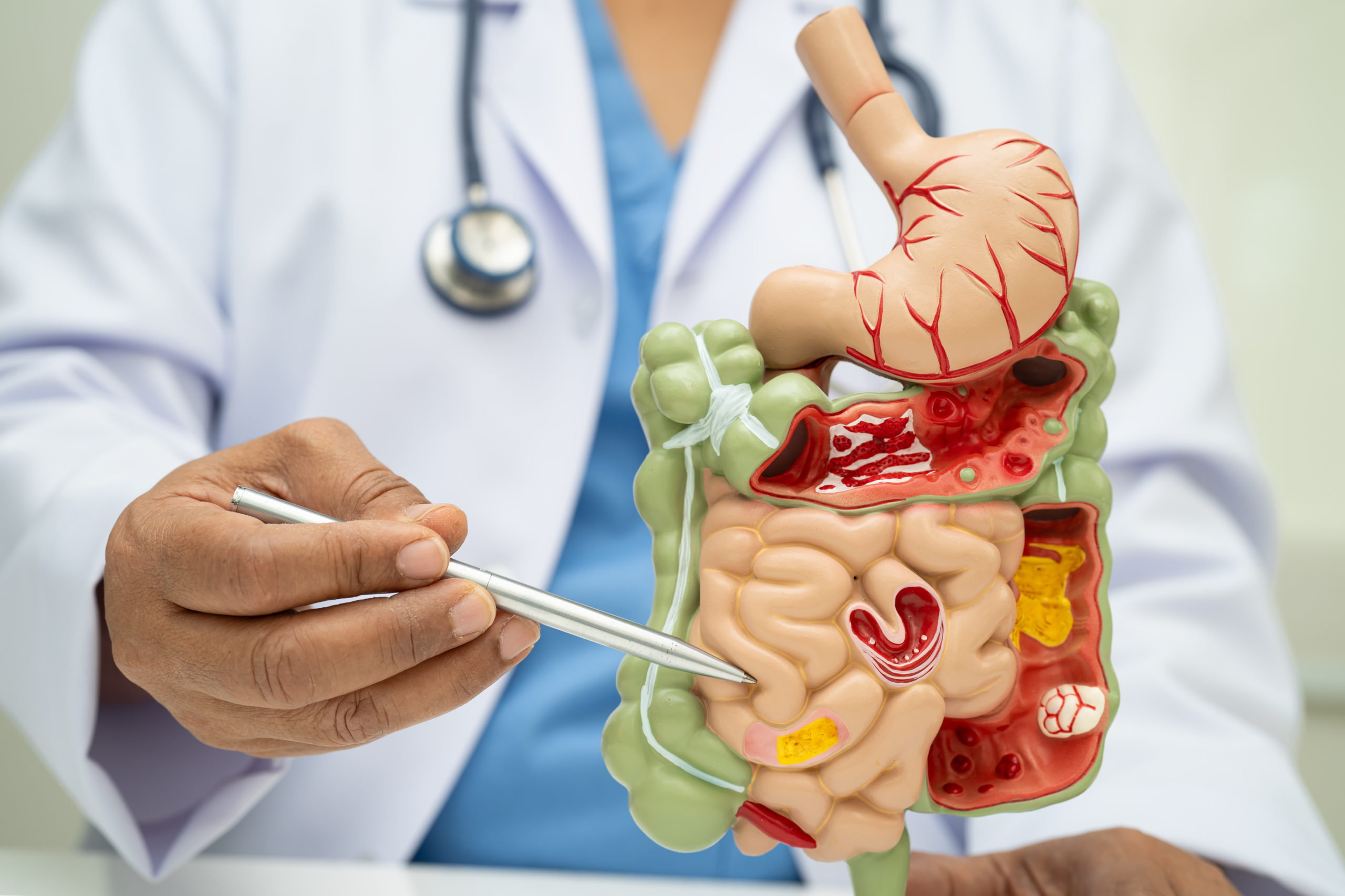
You’ve likely heard that fiber benefits digestive health, but do you know why? The answer lies in short-chain fatty acids (SCFAs), particularly butyrate. This important compound frequently appears in discussions on colon function and cellular energy metabolism.
This article explores butyrate’s role in maintaining a balanced gut, its production process, and practical ways to enhance its levels for optimal digestive health.
What Is Butyrate?
Butyrate, also called butyric acid, forms in the lower digestive tract when specific gut bacteria break down dietary fiber. This fermentation process generates various SCFAs, such as acetate, propionate, and butyrate, which support gut health. Among these, butyrate stands out as a crucial energy source for cells lining the large intestine.
- How butyrate is formed — When you consume fiber-rich foods like fruits, vegetables, and legumes, the fiber passes through the upper digestive tract largely intact. Once it reaches the colon, bacteria such as Roseburia and Faecalibacterium ferment the fiber, producing SCFAs.
- Butyrate fuels colon cells — Cells in the colon, known as colonocytes, rely on SCFAs for energy, with butyrate playing a particularly significant role. It is converted into acetyl-CoA, which then fuels the Krebs cycle in mitochondria, producing ATP—the fundamental energy currency for cellular activities.
- Colonocytes rely heavily on butyrate — Studies indicate that between 70% and 80% of the energy required by colonocytes comes from butyrate. When these cells receive a steady energy supply, they function optimally, maintaining digestive efficiency.
- Supports essential gut functions — Butyrate plays a role in fluid exchange and preserving the gut lining. Although individual dietary patterns may vary, research shows that colonocytes consistently rely on butyrate to sustain these vital processes.
For further insights into butyrate’s impact on health, check out “Understanding Butyrate—The Key to Optimal Health and Well-Being.”
Butyrate and Gut Barrier Integrity
The intestines, particularly the large intestine, act as a selective barrier, regulating what enters the bloodstream. SCFAs influence tight-junction proteins, which serve as gatekeepers in the intestinal lining.
- Strengthens gut barrier proteins — Proteins such as zonula occludens (ZO-1), occludin, and claudins play a critical role in gut integrity. Butyrate has been found to support their normal expression, enhancing intestinal barrier function.
- Encourages mucus production — The colon’s inner lining is coated with mucus, which facilitates waste movement and maintains a stable microbial environment. Healthy colon cells contribute to mucus production, and butyrate supports this process.
- Maintains anaerobic bacteria balance — As colonocytes metabolize butyrate, they consume oxygen, reducing oxygen levels in the colon. This low-oxygen environment supports anaerobic bacteria, which, in turn, produce more SCFAs, creating a positive cycle that fosters gut health.
Diet and Lifestyle Factors That Influence Butyrate Levels
One of the most effective ways to boost SCFA production is by consuming fiber-rich foods. Whole grains, fruits, vegetables, and legumes provide the necessary substrates for fermentation by gut bacteria.
- Consume diverse fiber sources — A mix of soluble and insoluble fiber enhances gut health, as different types of fiber support distinct microbial processes.
- Increase fiber intake gradually — If you are not accustomed to a high-fiber diet, sudden changes may cause bloating or discomfort. A slow increase allows your digestive system to adjust. Staying hydrated is also essential, as fiber without adequate fluid intake can lead to constipation.
- Limit polyunsaturated fats (PUFAs) — Diets high in PUFAs, especially those rich in linoleic acid from sources like soybean and corn oil, can negatively affect SCFA production. Reducing these fats supports a balanced gut microbiome.
- Exercise promotes microbial diversity — Physical activity contributes to a healthier gut by increasing microbiome diversity and improving digestion.
- Prioritize sleep and stress management — Sleep deprivation and chronic stress disrupt gut bacteria balance. Aiming for 7-8 hours of rest and adopting stress-reducing habits helps maintain a stable microbial environment.
- Be mindful of antibiotic use — Antibiotics impact both harmful and beneficial bacteria. After a course of antibiotics, replenishing the gut with probiotics and prebiotic-rich foods like yogurt, kefir, and fermented vegetables helps restore balance.
Making intentional dietary and lifestyle choices fosters an environment conducive to butyrate production, ultimately supporting digestive and overall health.
Debunking Common Butyrate Myths
Despite its importance, misconceptions about butyrate persist. Here are a few common misunderstandings:
- Fiber supplements are not a perfect substitute — While fiber supplements can be helpful, they do not fully replace the diversity and nutritional benefits of whole foods.
- Not all fats harm gut health — While processed fats and excessive linoleic acid can disrupt microbial balance, healthier fats such as grass-fed butter, ghee, and coconut oil support a gut-friendly diet when consumed in moderation.
- Protein alone does not damage the gut — A high-protein diet is only problematic if it lacks fiber. A balanced diet that includes quality protein sources alongside fiber-rich foods benefits gut health.
- Probiotics do not directly produce butyrate — Butyrate production depends on fiber-fermenting microbes. Some probiotics foster a favorable gut environment, but they do not directly generate butyrate.
Understanding these nuances empowers individuals to make informed choices that genuinely promote gut health.
Five Practical Strategies to Boost Butyrate Production
Increasing butyrate levels does not have to be complicated. Here are some simple and effective strategies:
- Eat fiber-rich foods — Berries, pears, and roasted vegetables provide both fiber and flavor.
- Avoid certain fibers if gut health is compromised — If experiencing severe gut issues, some fibers may need to be temporarily avoided to allow healing.
- Eliminate gut disruptors — Reducing exposure to linoleic acid, excess estrogen, and environmental stressors supports gut recovery.
- Start with low-fiber carbohydrates — In the initial healing phase, consuming low-fiber carbs can help rebalance the gut before gradually introducing more fiber.
Reintroduce fiber slowly — Once gut health improves, increasing fiber intake gradually supports the growth of SCFA-producing bacteria.